Back to 2025 Abstracts
Prehabilitation Reduces Non-Home Discharge After Esophagectomy in High-risk Esophageal Cancer Patients: A Pilot Study
Steven Tohmasi
*, Shaleen Sathe, Yifei Xu, Jingxia Liu, Jennifer Cook, Christina Kasting, Vanessa Curtis, Laura Carpenter, Melanie Koenen, Nikki Rossetti, Whitney S. Brandt, Varun Puri, Bryan F. Meyers, Dominic E. Sanford, Benjamin D. Kozower
Department of Surgery, Washington University School of Medicine, Saint Louis, MO
Objective: Esophagectomy is associated with significant morbidity. The benefits of prehabilitation, a strategy focused on optimizing physical and psychological well-being before surgery, on outcomes after esophagectomy remain unclear. This study evaluates the impact of a multidisciplinary preoperative prehabilitation program on postoperative outcomes in high-risk esophagectomy patients.
Methods: In 2021, our institution implemented a multidisciplinary, evidence-based prehabilitation program (Surgical Prehabilitation and Readiness: SPAR) for high-risk surgical patients targeting physical activity, pulmonary function, nutritional optimization, and mindfulness. Patients enrolled in SPAR from 2022 to 2024 who underwent esophagectomy for esophageal cancer were compared with historical control patients (pre-SPAR) from our institutional ACS National Surgical Quality Improvement Program (NSQIP) database who underwent esophagectomy during the 5 years prior to program implementation (2016-2020). SPAR patients were propensity score matched with pre-SPAR NSQIP patients in a 1:3 ratio and postoperative outcomes were compared using Wilcoxon rank sum test and Fisher's exact test.
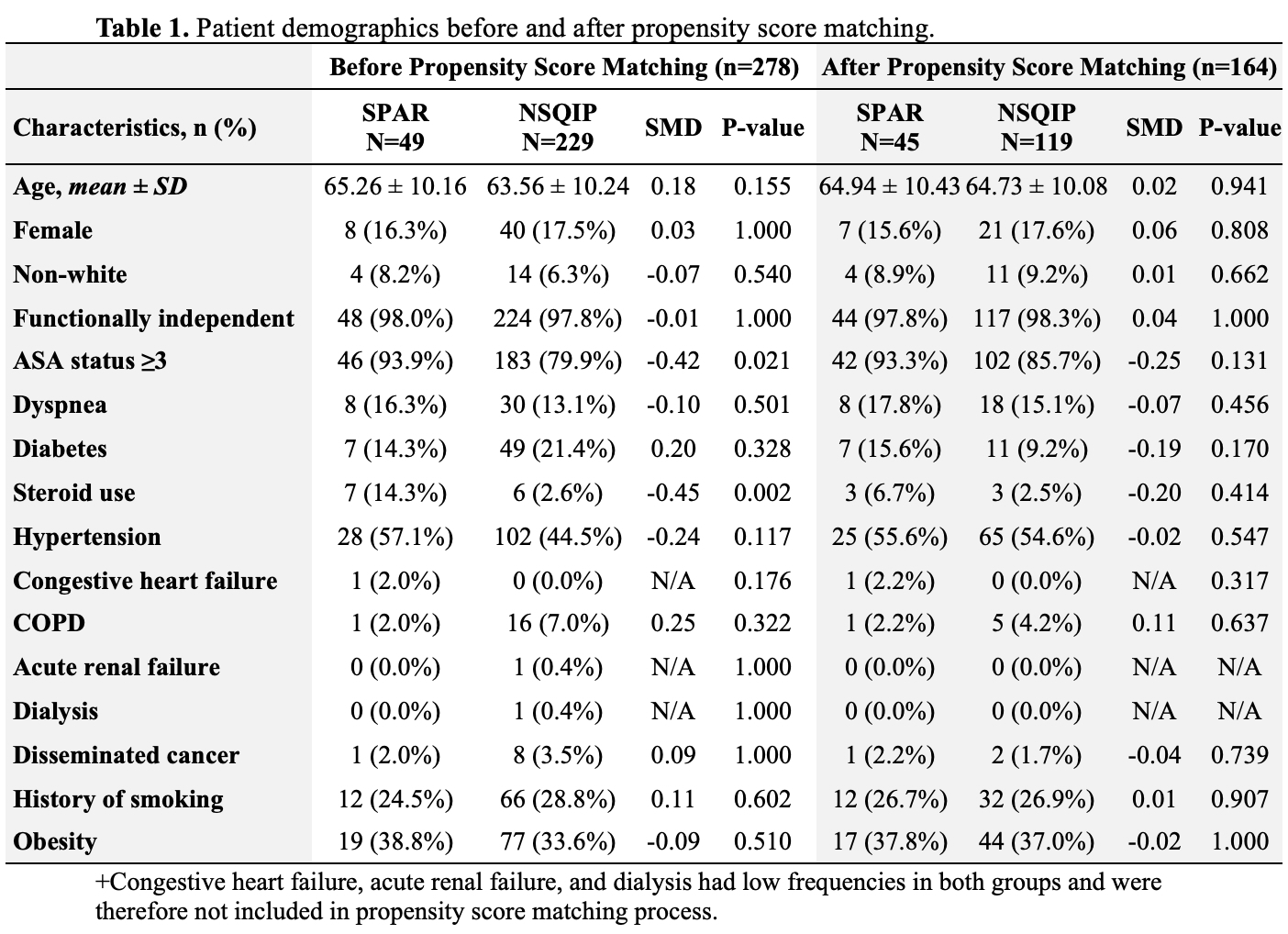
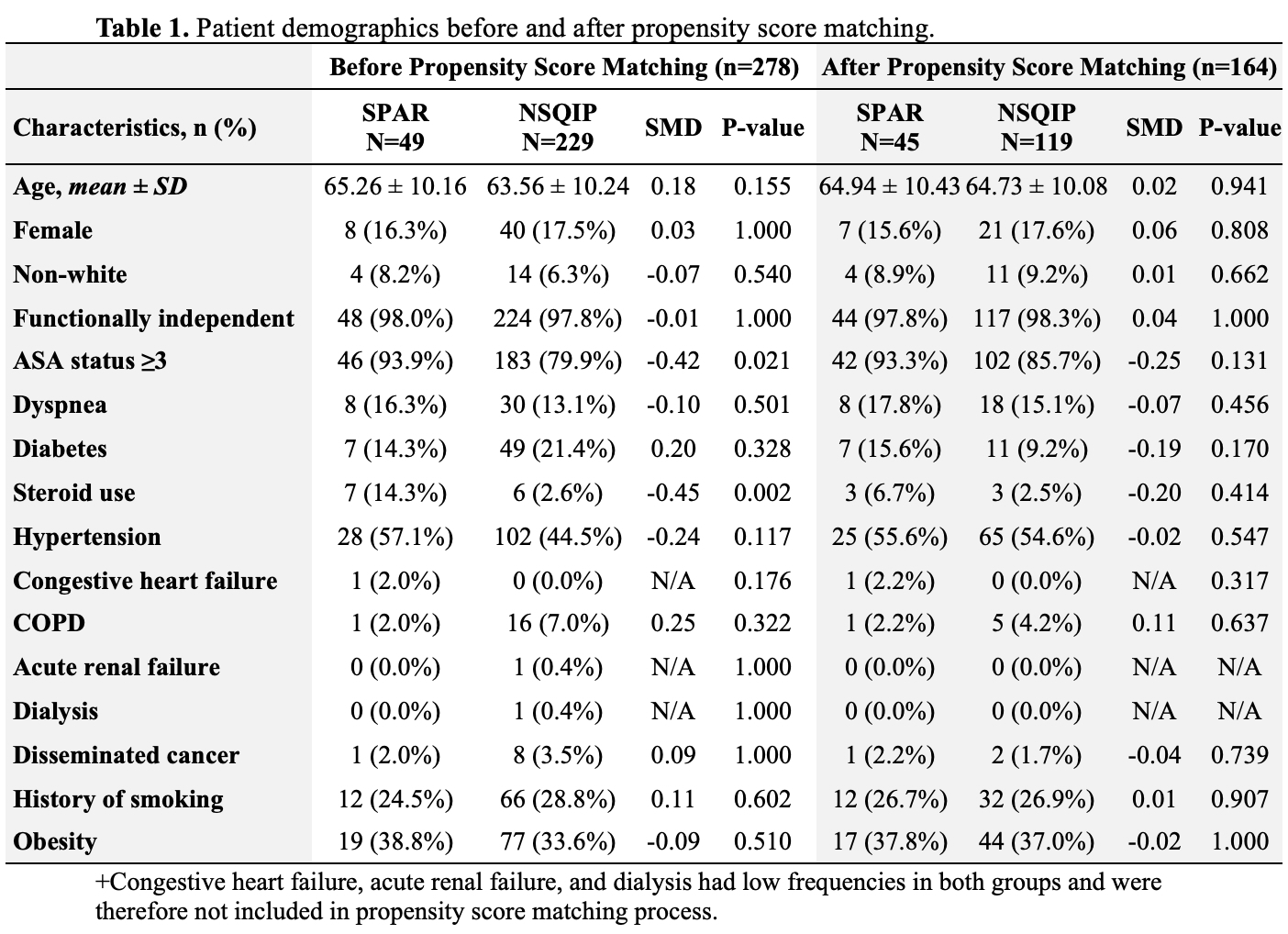
Results: In total, 49 SPAR and 229 pre-SPAR NSQIP patients underwent esophagectomy, with 30-day follow-up data available. At baseline, SPAR patients were significantly more likely to have severe systemic disease (American Society of Anesthesiologists class ≥3: 93.9% vs. 79.9%, p=0.021) and chronic steroid use (14.3% vs. 2.6%, p=0.002), compared to pre-SPAR NSQIP patients. Of the 49 SPAR patients, 45 patients (91.8%) were propensity score matched to 119 pre-SPAR NSQIP patients (Table 1). After propensity score matching, SPAR patients had significantly lower rates of discharge to post-acute care facilities (4.4% vs 16.8%, p=0.039) but similar 30-day mortality (4.4% vs. 0.8%, p=0.096), 30-day readmission rates (6.7% vs. 8.4%, p=0.873), and hospital length of stay (12.6 ±10.4 vs. 11.4 ±5.6 days, p=0.164), compared to pre-SPAR NSQIP patients.
Conclusions: Participation in a structured prehabilitation program before esophagectomy may reduce the need for non-home discharge and help preserve functional independence in high-risk esophageal cancer patients. Future research should examine longer-term functional outcomes and health-related quality of life measures to better define the impact of prehabilitation on patient outcomes following esophagectomy.
Back to 2025 Abstracts